New technology cures GERD without surgery is revolutionizing the way we approach Gastroesophageal Reflux Disease (GERD). Current treatments often involve lifestyle changes, medications, or even surgery, each with its own limitations and potential side effects. This innovative approach promises a less invasive and potentially more effective path to relief, offering hope for those seeking GERD solutions without the need for surgical intervention.
This article explores the emerging technologies addressing GERD, examining their potential mechanisms of action, clinical trial considerations, patient acceptance, cost-effectiveness, potential risks, regulatory hurdles, and future research directions. A comparative analysis with existing surgical procedures will further illuminate the advantages and disadvantages of each treatment approach.
Introduction to GERD and Current Treatments
Gastroesophageal reflux disease (GERD) is a chronic digestive disorder characterized by the backward flow of stomach acid into the esophagus. This acidic reflux can irritate the esophageal lining, leading to symptoms like heartburn, regurgitation, and chest pain. While GERD is a common condition, its impact on quality of life can be significant.Current treatments for GERD encompass a range of approaches, from lifestyle modifications to pharmaceutical interventions, and in some cases, surgical procedures.
Understanding the limitations and potential side effects of these treatments is crucial for patients to make informed decisions regarding their care.
Common Treatments for GERD
Lifestyle modifications are often the first line of defense in managing GERD symptoms. These adjustments can include dietary changes (avoiding trigger foods like fatty or spicy foods, chocolate, caffeine, and alcohol), weight management, elevating the head of the bed, and avoiding tight-fitting clothing. These measures aim to reduce the frequency and severity of acid reflux.Medications are also commonly prescribed to treat GERD.
Antacids provide temporary relief from heartburn by neutralizing stomach acid. H2 blockers reduce the production of stomach acid, offering longer-lasting relief. Proton pump inhibitors (PPIs) are the most potent class of acid-suppressing medications, significantly reducing acid production.
Limitations and Potential Side Effects of Current Treatments
While effective in managing symptoms, current GERD treatments can have limitations and potential side effects. Lifestyle modifications, while generally safe, may not be sufficient for all patients. Medications, particularly long-term use of PPIs, can increase the risk of certain side effects like vitamin B12 deficiency, Clostridium difficile infection, and bone fractures. Surgical interventions, though sometimes necessary, carry their own set of risks and potential complications.
Comparison of GERD Treatment Options
| Treatment Option | Effectiveness Rating | Side Effects | Cost | Patient Compliance |
|---|---|---|---|---|
| Lifestyle Modifications | Moderate (variable based on individual response) | Generally minimal, but some individuals may find it challenging to adhere to dietary restrictions. | Low | High (if well-supported) |
| Antacids | Low (temporary relief) | Generally mild, but can cause constipation or diarrhea in some individuals. | Low | Moderate (due to frequent use) |
| H2 Blockers | Moderate (longer-lasting relief than antacids) | Generally mild, but can cause headaches, dizziness, and diarrhea in some individuals. | Moderate | Moderate (daily use) |
| Proton Pump Inhibitors (PPIs) | High (effective in reducing acid production) | Increased risk of vitamin B12 deficiency, Clostridium difficile infection, bone fractures, and kidney problems with long-term use. | Moderate to High | Moderate (daily use and potential for long-term use) |
| Surgical Procedures (e.g., fundoplication) | High (long-term solution for severe GERD) | Risks of infection, bleeding, and difficulty swallowing (dysphagia). Longer recovery period. | High | High (long-term solution) |
Emerging Technologies for GERD Management
Innovative approaches to managing gastroesophageal reflux disease (GERD) are constantly evolving, moving beyond traditional therapies toward minimally invasive and targeted solutions. These emerging technologies aim to address the limitations of existing treatments, such as medication side effects and the need for surgical intervention in certain cases. This section will explore some of these promising advancements.
Targeted Drug Delivery Systems
Novel drug delivery systems are being developed to enhance the effectiveness and safety of GERD medications. These systems aim to deliver the medication directly to the affected area in the esophagus and stomach, minimizing systemic side effects and maximizing therapeutic efficacy. One example is the use of nanoparticles, which can be designed to release the medication at a specific rate and location, ensuring optimal concentration at the site of action.
This approach is also being explored to enhance the absorption of existing GERD medications. These advancements have the potential to improve treatment outcomes while reducing the need for high doses of medication.
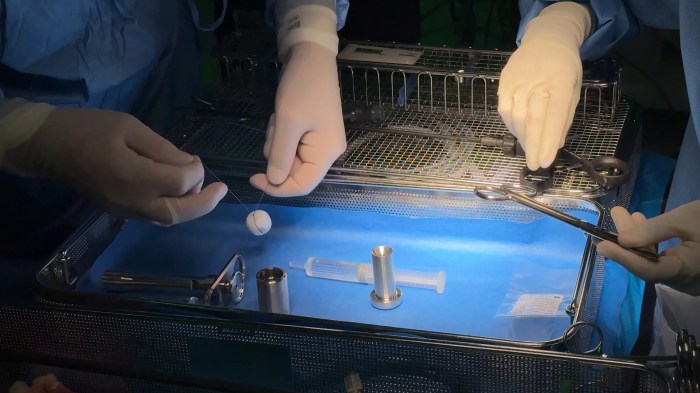
Endoscopic Technologies
Advancements in endoscopy are leading to more precise and less invasive treatment options for GERD. Endoscopic procedures, which utilize specialized tools inserted through the mouth, can now be used to target specific areas of reflux and repair damaged tissue. One example is the use of radiofrequency ablation, which can reduce esophageal inflammation and improve reflux control. Another example is the deployment of targeted therapies to treat reflux-related conditions such as Barrett’s esophagus, a precancerous condition.
These technologies are also paving the way for early diagnosis and surveillance of GERD complications.
Biofeedback and Neuromodulation Techniques
Biofeedback and neuromodulation approaches are emerging as promising non-invasive strategies for managing GERD. These techniques aim to regulate the function of the esophageal sphincter, which controls the opening between the esophagus and stomach. For instance, biofeedback systems can provide real-time feedback to patients, allowing them to learn to control their esophageal muscle activity and reduce reflux episodes. Neuromodulation, using electrical or chemical stimulation, can also influence the function of the esophageal sphincter, potentially improving reflux control.
These approaches hold potential for long-term management and symptom reduction, without the need for medication or surgery.
Comparison of Emerging Technologies
| Technology Type | Mechanism of Action | Efficacy | Safety Concerns | Cost |
|---|---|---|---|---|
| Targeted Drug Delivery Systems | Deliver medication directly to the affected area, minimizing systemic side effects. | High potential for improved efficacy and reduced side effects. Clinical trials are ongoing. | Potential for unforeseen side effects related to the delivery system. Requires careful design and testing. | Likely higher than traditional medications due to the complexity of the formulation and manufacturing. |
| Endoscopic Technologies | Utilize specialized tools to target and treat reflux-related issues. | High efficacy in addressing specific reflux issues. Established safety profile for endoscopic procedures. | Potential for complications associated with any endoscopic procedure, such as bleeding or perforation. | Generally higher than medication-based treatments, but lower than surgical procedures. |
| Biofeedback and Neuromodulation | Regulate esophageal sphincter function through patient feedback or electrical/chemical stimulation. | Promising results in reducing reflux episodes and improving symptoms. | Potential for discomfort or mild side effects during stimulation procedures. | Potentially lower than other therapies due to less complex procedures. |
Potential Mechanisms of Action for New Technologies
Novel technologies aimed at alleviating GERD symptoms operate on diverse principles, potentially targeting multiple aspects of the disease process. Understanding these mechanisms is crucial for evaluating the efficacy and safety of these interventions. By addressing the underlying physiological factors, these approaches offer a promising avenue for non-surgical GERD management.
Potential Mechanisms of Acid Reduction
Several emerging technologies are exploring methods to reduce stomach acid production. These strategies may involve modulating the activity of the parietal cells, which are responsible for secreting hydrochloric acid. One potential approach utilizes targeted drug delivery systems, delivering medications directly to the parietal cells to inhibit acid production, while minimizing systemic side effects. Another avenue involves the use of bioengineered compounds that specifically bind to and neutralize acid in the stomach.
The goal is to achieve a more neutral pH, thus minimizing the corrosive effects of stomach acid on the esophageal lining.
Mechanisms for Strengthening Esophageal Muscles
Esophageal motility disorders contribute significantly to GERD symptoms. Technologies focused on strengthening esophageal muscles aim to improve the lower esophageal sphincter (LES) function and esophageal motility. This could involve electrical stimulation of the esophageal muscles, which can strengthen contractions and prevent reflux. Alternatively, bioengineered scaffolds could be implanted in the esophagus to provide structural support and improve its mechanical strength, thereby enhancing the LES function and preventing reflux episodes.
Mechanisms for Improving Esophageal Motility
Technologies targeting esophageal motility dysfunction aim to restore normal esophageal contractions and transit. These approaches could involve the use of targeted neuromodulators to stimulate the nerves controlling esophageal muscle contractions, thus promoting faster and more efficient esophageal transit. Moreover, novel therapies may utilize electrical stimulation to enhance peristaltic waves and prevent the accumulation of stomach contents in the esophagus.
These technologies can be tailored to address specific motility patterns observed in GERD patients.
Altering the Stomach Acid Environment
Some technologies are designed to directly alter the environment within the stomach. This may involve delivering compounds that can neutralize stomach acid or buffer its corrosive effects. Additionally, some strategies may target the bacterial populations within the stomach to reduce the production of substances that promote acid secretion.
Illustrative Mechanism of Action Diagram (Example: Targeted Drug Delivery System)
| Component | Description | Mechanism |
|---|---|---|
| Drug Carrier | A biocompatible polymer or microparticle designed to release a specific medication. | Delivers the drug directly to parietal cells. |
| Targeted Drug | A medication that specifically inhibits acid production in parietal cells. | Blocks acid secretion. |
| Parietal Cell | A stomach cell responsible for producing hydrochloric acid. | Targeted for drug delivery and acid reduction. |
| Stomach Acid | Hydrochloric acid produced in the stomach. | Reduced through the action of the targeted drug. |
Note: This diagram illustrates a simplified example. Actual mechanisms may involve more complex interactions.
Clinical Trials and Research
Evaluating new GERD treatments necessitates rigorous clinical trials to assess efficacy and safety. These trials provide crucial data for regulatory approval and ultimately, patient benefit. Successful trials establish the treatment’s effectiveness compared to existing methods or a placebo, and identify potential side effects.
Types of Clinical Trials
A variety of clinical trial designs are employed to rigorously evaluate the efficacy and safety of new GERD technologies. These include randomized controlled trials (RCTs), which compare the new technology to a standard treatment or a placebo, ensuring unbiased results. Observational studies, while valuable for initial exploration, are not as definitive in establishing cause-and-effect relationships. Phase I trials focus on safety, dosage, and tolerability in a small group of participants.
Phase II trials evaluate efficacy and further refine safety profiles in a larger group. Phase III trials compare the new technology to existing standards, confirming effectiveness and further assessing safety in a large, diverse population. Phase IV trials continue to monitor long-term effects and rare side effects in the post-market setting.
Recent breakthroughs in new technology are offering promising cures for GERD without surgery. Researchers are exploring innovative approaches, including the application of new microwave technology for targeted thermal therapies. This novel approach shows potential for effectively treating GERD without the need for invasive procedures.
Key Metrics and Outcome Measures
Precise measurements are critical for evaluating GERD treatments. Key metrics include the frequency and severity of GERD symptoms, such as heartburn, regurgitation, and chest pain, as assessed by validated questionnaires and symptom diaries. Objective measures, like esophageal pH monitoring and impedance measurements, provide more quantifiable data on acid reflux events. Quality of life assessments are also essential, evaluating how the treatment impacts daily activities and overall well-being.
These outcome measures, when combined, provide a comprehensive picture of the treatment’s impact. For example, a significant reduction in heartburn episodes as measured by pH monitoring, coupled with improved quality of life scores, suggests a positive treatment outcome.
Study Protocol Design
A well-structured study protocol is crucial for a clinical trial’s success. This document details the entire trial process, including participant selection criteria, intervention procedures, data collection methods, and statistical analysis plans. A key element is the randomization process, ensuring that participants are assigned to treatment groups (new technology or control) randomly, minimizing bias. For instance, a study evaluating a new endoscopic device for GERD treatment would specify inclusion criteria (e.g., age, severity of GERD, lack of response to existing treatments), the device’s application protocol, the frequency of follow-up visits, and the specific outcome measures.
The protocol should also address potential adverse events and how they will be managed.
Ethical Considerations and Patient Safety Regulations
Ethical considerations are paramount in clinical trials. Informed consent is absolutely essential, ensuring participants fully understand the trial’s purpose, procedures, potential risks, and benefits. Independent ethics committees (IECs) review the trial protocol to ensure ethical conduct and patient safety. Data privacy and confidentiality are also critical, with strict adherence to regulations like HIPAA in the US. For instance, patient data must be securely stored and accessed only by authorized personnel.
Safety monitoring throughout the trial is essential, allowing early detection and management of adverse events. Safety regulations, like those mandated by the FDA (Food and Drug Administration), must be followed meticulously.
Regulatory Approval Process
Obtaining regulatory approval for a new GERD treatment is a multi-step process. The process typically involves submitting detailed data from clinical trials to regulatory bodies like the FDA (US) or EMA (European Union). This includes detailed study protocols, participant data, and safety analyses. Regulatory review involves rigorous scrutiny to ensure the treatment’s safety and efficacy meet predefined standards.
Subsequent approvals, if granted, allow the treatment to be marketed and sold legally. This process can take several years, but the meticulous evaluation helps ensure patient safety and the treatment’s value. For instance, a new device designed for minimally invasive GERD treatment would need to meet specific performance standards and safety criteria set by the regulatory agencies.
Patient Experience and Acceptance
Patients with gastroesophageal reflux disease (GERD) often face a range of symptoms, significantly impacting their quality of life. The desire for effective, non-invasive treatments is paramount. Understanding patient perceptions and preferences for emerging technologies is crucial for successful adoption and improved outcomes.A comprehensive approach to evaluating patient acceptance must consider factors beyond just the technical efficacy of the technology.
Psychological, social, and practical considerations all play a vital role in how patients perceive and ultimately utilize new treatments. This section will delve into these key factors, presenting potential strategies for improved patient engagement.
Patient Perceptions of Non-Surgical GERD Treatments
Patients’ perceptions of new GERD technologies are influenced by various factors. These include prior experiences with medical treatments, perceived risks and benefits, and the ease of use and convenience of the technology. Positive patient experiences with similar technologies in other medical contexts can foster trust and encourage adoption. Conversely, negative experiences or concerns about side effects or invasiveness can hinder acceptance.
Factors Influencing Patient Acceptance
Several key factors influence a patient’s willingness to adopt a new medical treatment. These include perceived effectiveness, safety profile, ease of use, and the overall cost of treatment. Additionally, factors like the patient’s age, cultural background, and access to healthcare resources play a role. Understanding these diverse influences is crucial for tailoring patient engagement strategies.
Examples of Successful Patient Engagement Strategies
Successful patient engagement in clinical trials and other healthcare contexts frequently involve clear communication, active listening, and a focus on patient empowerment. Providing patients with comprehensive information about the technology, including potential benefits and risks, is essential. Regular feedback mechanisms and opportunities for patients to voice concerns and preferences further strengthen trust and acceptance. Patient advisory boards, where patients actively participate in the design and implementation of treatment strategies, are highly effective.
Survey Questionnaire for Assessing Patient Preferences
This questionnaire is designed to gather insights into patient preferences for new GERD treatments.
| Question | Type | Possible Responses |
|---|---|---|
| What is your current level of satisfaction with your GERD treatment? | Rating scale (1-5) | 1=Very Dissatisfied, 5=Very Satisfied |
| How important is a non-surgical approach to GERD treatment for you? | Rating scale (1-5) | 1=Not at all important, 5=Extremely important |
| How comfortable would you be with a new GERD treatment that does not require surgery? | Rating scale (1-5) | 1=Very Uncomfortable, 5=Very Comfortable |
| Would you be willing to participate in a clinical trial for a new non-surgical GERD treatment? | Yes/No | Yes, No |
| What are your primary concerns about new GERD treatments? | Open-ended | Free-form response |
| How important is ease of use for a GERD treatment? | Rating scale (1-5) | 1=Not at all important, 5=Extremely important |
| How important is the potential for side effects for a GERD treatment? | Rating scale (1-5) | 1=Not at all important, 5=Extremely important |
Improving Patient Communication
Effective communication about new technologies is crucial for fostering patient trust and acceptance. Clear, concise explanations of the technology, its potential benefits and risks, and the process involved in its use are vital. Using visuals, analogies, and relatable examples can further enhance understanding. Regular updates and feedback mechanisms can address any concerns or questions that may arise.
Cost-Effectiveness Analysis: New Technology Cures Gerd Without Surgery
Assessing the financial viability of new non-surgical GERD treatments is crucial for their widespread adoption. This involves evaluating the potential costs of implementation, comparing their cost-effectiveness against existing treatments, and projecting long-term economic implications. Understanding the return on investment for these novel technologies is paramount for healthcare providers and payers alike.
Potential Costs of Implementation
Implementing new technologies involves various costs, including research and development, manufacturing, regulatory approvals, training for healthcare professionals, and the acquisition of necessary equipment. The initial investment can be substantial, but the long-term benefits must outweigh these costs. Factors such as the complexity of the technology and the scale of production will significantly influence the overall cost. Similar to the rollout of any new medical device, careful planning and budgeting are essential to ensure the financial sustainability of the program.
Comparison to Existing Treatments
Comparing the cost-effectiveness of new technologies to existing GERD treatments necessitates a comprehensive evaluation of both short-term and long-term costs. This includes direct costs such as medication expenses and procedures, as well as indirect costs such as lost productivity and quality of life impacts. Consideration should be given to the potential for reduced healthcare resource utilization in the long run.
For instance, if a new technology reduces the need for follow-up appointments or surgery, the long-term cost savings can be substantial.
Long-Term Economic Implications, New technology cures gerd without surgery
Adopting new GERD technologies has significant long-term implications for healthcare systems and patients. Potential benefits include reduced healthcare costs, improved patient outcomes, and enhanced quality of life. However, potential challenges include the need for ongoing maintenance, potential for complications, and the need for long-term follow-up care. The economic impact will be multifaceted and require careful monitoring to ensure the benefits outweigh the costs.
Examples of Cost-Benefit Analyses in Similar Medical Contexts
Cost-effectiveness analyses are frequently used in medical contexts to assess the value of new technologies. For example, the adoption of minimally invasive surgical techniques in various specialties demonstrated a significant reduction in hospital stays and recovery times, resulting in substantial cost savings. Similar analyses can be applied to new GERD technologies, evaluating the cost of treatment against the potential for reduced long-term healthcare costs.
Studies examining the cost-effectiveness of various cancer treatments, for instance, provide useful frameworks for similar analyses in GERD.
Projected Costs and Benefits of a Hypothetical Technology
| Cost Component | Estimated Cost (USD) | Benefit (e.g., Reduced Surgery Rate) |
|---|---|---|
| Research and Development | $10,000,000 | Reduction in GERD-related hospitalizations |
| Manufacturing and Supply Chain | $5,000,000 per year | Reduction in chronic pain |
| Regulatory Approval | $2,000,000 | Improved patient quality of life |
| Healthcare Professional Training | $1,000,000 | Reduced need for long-term medication |
| Initial Equipment Purchase | $100,000 per facility | Faster recovery times |
| Total Initial Investment | $18,100,000 | Overall positive impact on healthcare system |
| Annual Treatment Cost | $500-$1000 per patient | Improved treatment compliance |
| Long-Term Savings (e.g., Reduced Surgery) | $1,000-$5,000 per patient | Improved patient outcomes |
This table presents a simplified example of potential costs and benefits associated with a hypothetical new GERD treatment. Actual figures will vary depending on the specific technology and its implementation context. These figures illustrate the importance of considering both initial investment and long-term savings in evaluating cost-effectiveness.
Potential Risks and Side Effects
While these innovative technologies hold promise for revolutionizing GERD treatment, potential risks and side effects are inherent in any new medical intervention. Thorough investigation and rigorous testing are crucial to understanding and mitigating these risks, ensuring patient safety and the long-term efficacy of these treatments.A comprehensive assessment of potential adverse events is paramount. This includes not only immediate reactions but also the possibility of long-term consequences.
Careful consideration of these factors will be critical in shaping the responsible adoption and implementation of these new technologies.
Potential Adverse Events
Careful investigation into potential adverse events is essential to ensure the safety and efficacy of new technologies. This includes considering both short-term and long-term consequences, as well as the potential for individual patient variations in response. Understanding these variables will aid in developing strategies to mitigate the risks and ensure the best possible outcomes for patients.
Importance of Rigorous Testing
Minimizing potential risks necessitates robust pre-clinical and clinical trials. These trials should employ diverse patient populations to assess the efficacy and safety across a broader spectrum of individuals. Rigorous data collection, analysis, and reporting are crucial to identifying any potential adverse events, no matter how infrequent. This proactive approach ensures the responsible advancement of these therapies.
Potential Long-Term Consequences
Long-term consequences are a significant concern in evaluating any new technology. Studies must extend beyond short-term observations to identify any potential long-term effects on the body’s systems. Considering the potential for chronic effects, including organ function or other physiological systems, is paramount to a thorough risk assessment.
Strategies for Mitigating Side Effects
Developing strategies to mitigate side effects is critical. This includes establishing clear protocols for patient monitoring, proactive management of potential complications, and the development of treatment protocols for adverse events. These proactive measures ensure patient safety and support the responsible advancement of these therapies.
Table of Known and Potential Risks
| Risk | Severity | Preventative Measures |
|---|---|---|
| Localized inflammation at the treatment site | Mild to Moderate | Careful selection of treatment site, optimized dosage, and regular monitoring. |
| Gastrointestinal discomfort (e.g., nausea, bloating) | Mild to Moderate | Adjusting treatment parameters, providing supportive care, and educating patients about potential symptoms. |
| Systemic allergic reactions | Moderate to Severe | Pre-treatment allergy testing, close monitoring during treatment, and having emergency protocols in place. |
| Interactions with other medications | Variable | Thorough medication history review, appropriate drug interaction analysis, and close monitoring for adverse effects. |
| Unforeseen long-term effects on esophageal motility | Unknown | Long-term follow-up studies, continuous monitoring, and ongoing research into potential long-term complications. |
Regulatory Landscape

Navigating the regulatory landscape is crucial for any new medical technology. The process is complex, demanding rigorous scientific evidence and adherence to established guidelines. Understanding these intricacies is vital for the successful development and eventual implementation of these groundbreaking GERD treatments.
Regulatory Pathways for New Technologies
The FDA (Food and Drug Administration) in the US, and equivalent regulatory bodies globally, oversee the approval of new medical devices and therapies. The specific pathway depends on the classification of the technology, ranging from low-risk devices requiring less stringent review to high-risk ones needing more extensive testing and data. These classifications typically assess the invasiveness and potential for adverse effects of the technology.
Challenges and Opportunities for Regulatory Approval
Securing regulatory approval for novel GERD treatments presents both hurdles and opportunities. The rigorous scientific requirements and extensive clinical trial demands can be time-consuming and resource-intensive. However, successful approval paves the way for widespread adoption and significantly improves patient access to innovative therapies.
Examples of Successful Regulatory Approvals for Similar Medical Innovations
Several successful approvals for medical innovations in related areas provide valuable insight. For instance, the approval of minimally invasive surgical techniques, or advanced endoscopic tools, demonstrates the regulatory pathway’s capacity to assess and approve innovative medical procedures. These examples underscore the importance of rigorous clinical trial data in securing regulatory approval. Furthermore, the approvals for various drug therapies highlight the scrutiny and data requirements for new pharmacological interventions.
Steps Involved in the Regulatory Approval Process
The regulatory approval process typically involves several key steps. First, a pre-clinical assessment evaluates the safety and efficacy of the technology. Second, well-designed clinical trials are crucial to demonstrate the effectiveness and safety in humans. Third, comprehensive documentation of the entire process, including detailed research and data analysis, is submitted to the regulatory body. Finally, a rigorous review process by the regulatory authority assesses the submitted data, and a decision is made regarding approval or denial.
Successful completion of these steps is essential for market authorization.
Legal Considerations Related to the Use of New Technologies
Legal considerations, including intellectual property rights, liability, and patient rights, are paramount. A clear understanding of these legal implications is essential for developing the technology while safeguarding against potential issues. For instance, intellectual property rights and their protection are vital, as are the provisions and regulations regarding patient data and confidentiality.
Future Directions and Research Priorities
The burgeoning field of non-surgical GERD treatments necessitates a proactive approach to future research. Continued advancements in technology offer promising avenues for developing effective and minimally invasive therapies, potentially revolutionizing patient care. This section Artikels key areas for future research, emphasizing multidisciplinary collaboration and long-term implications.
Promising Research Areas
Further investigation into the underlying mechanisms of GERD is crucial for developing targeted therapies. Researchers should explore novel approaches to address the complex interplay of factors contributing to acid reflux, such as esophageal motility disorders, impaired sphincter function, and dietary influences. This includes studying the impact of specific dietary components on esophageal pH and motility, and identifying biomarkers for early detection and personalized treatment strategies.
This multi-pronged approach will lead to a deeper understanding of GERD and a more nuanced approach to treatment.
Multidisciplinary Collaboration
Successful development of non-surgical GERD treatments demands a collaborative effort among various disciplines. This includes gastroenterologists, engineers, pharmacists, and biomedical researchers. Collaboration fosters the exchange of expertise, enabling researchers to leverage insights from diverse perspectives. Cross-disciplinary teams can efficiently tackle the multifaceted challenges of GERD, promoting the development of innovative and effective therapies. Examples include interdisciplinary teams designing and testing novel drug delivery systems, and researchers from engineering backgrounds contributing to the development of novel endoscopic devices.
Long-Term Implications
Advancements in non-surgical GERD treatments could have significant long-term implications for patient care. Improved treatment options could lead to a reduction in the need for invasive procedures, reducing patient discomfort and healthcare costs. Reduced reliance on surgery may also lessen the potential for complications associated with surgical interventions, leading to better long-term outcomes for patients. Ultimately, this translates into enhanced patient quality of life and a more cost-effective approach to managing GERD.
Key Research Focus Areas
This section highlights key areas for future research, focusing on the development of new and improved non-surgical GERD therapies. The areas are categorized to facilitate focused and targeted research efforts.
- Targeted Drug Delivery Systems: Developing novel drug delivery systems that can effectively target the esophageal mucosa and minimize systemic side effects. Examples include micro- or nano-encapsulated drugs, or smart drug delivery systems that respond to specific pH changes.
- Endoscopic Technologies: Exploring the application of advanced endoscopic technologies for precise targeting and treatment of GERD. This includes endoscopic mucosal resection (EMR) and endoscopic mucosal dissection (ESD) techniques. The goal is to create precise treatment options for patients with specific anatomical characteristics or complications.
- Bioengineered Treatments: Exploring the use of bioengineered tissues or cells to repair or reinforce the esophageal lining. This includes the development of novel regenerative therapies, which could potentially repair damaged esophageal tissue.
- Personalized Medicine: Developing personalized treatment strategies based on individual patient characteristics, including genetic predisposition, lifestyle factors, and the severity of GERD. This involves creating a tailored approach to treatment based on specific patient needs and characteristics.
Roadmap for Future Development
A roadmap for future development of non-surgical GERD treatments should be characterized by a phased approach. The initial phase should focus on preclinical testing and proof-of-concept studies, followed by rigorous clinical trials to validate efficacy and safety. The subsequent phases should involve refining treatment protocols and addressing specific patient needs. This should culminate in the development of accessible, affordable, and widely applicable non-surgical treatments for GERD.
- Phase 1: Fundamental research, preclinical studies, and proof-of-concept trials to assess the feasibility and potential of novel technologies.
- Phase 2: Pilot clinical trials to evaluate the safety and efficacy of the selected technologies in a small group of patients.
- Phase 3: Large-scale clinical trials to confirm the efficacy, safety, and long-term outcomes of the technologies in a broader patient population.
- Phase 4: Post-market surveillance and refinement of treatment protocols to address specific patient needs and optimize outcomes.
Comparison with Surgical Procedures
Non-surgical treatments for gastroesophageal reflux disease (GERD) are increasingly prevalent, offering an alternative to traditional surgical approaches. This section analyzes the comparative efficacy and safety profiles of these emerging technologies against established surgical interventions, highlighting the situations where surgery remains the preferred option.Surgical interventions, such as fundoplication, have been the gold standard for GERD management for decades. However, the development of minimally invasive and targeted non-surgical techniques presents a compelling alternative for many patients.
The choice between these approaches hinges on individual patient factors, treatment goals, and the specific nature of their GERD.
Efficacy and Safety Profiles
Non-surgical treatments often demonstrate comparable efficacy to surgical procedures in managing GERD symptoms, particularly in milder cases. These newer technologies aim to address the underlying mechanisms causing reflux, potentially offering long-term symptom control. However, surgical procedures typically offer a more definitive and permanent resolution, although this can be associated with a higher risk of certain complications. Long-term data on the efficacy and safety of non-surgical approaches is still accumulating, and ongoing research is crucial to fully assess their long-term impact.
Situations Favoring Surgical Interventions
Despite the rise of non-surgical options, surgical interventions remain a valuable treatment choice in specific situations. These include cases with severe or refractory GERD, where non-surgical treatments have proven insufficient, or in individuals with significant anatomical abnormalities impacting reflux control. Additionally, patients with severe complications from GERD, such as Barrett’s esophagus or esophageal strictures, may benefit from the more definitive approach surgery offers.
Patient Populations Benefiting from Non-Surgical Treatments
Non-surgical GERD treatments are well-suited for a broad range of patients. Individuals with mild to moderate GERD symptoms, those who are not good candidates for surgery due to health conditions or preferences, or those seeking less invasive options may find significant relief with these emerging technologies. This patient group encompasses a wide spectrum of ages and comorbidities. For instance, patients with significant anxiety regarding surgery or those with other medical conditions that preclude general anesthesia may be prime candidates for non-surgical approaches.
Comparison Table
| Characteristic | Non-Surgical Treatments | Surgical Procedures (e.g., Fundoplication) |
|---|---|---|
| Success Rates (estimated) | 70-85% (depending on specific technology and severity) | 80-90% (based on established studies) |
| Complications | Generally lower, often localized and temporary | Potential for complications such as bleeding, infection, or difficulty swallowing (though typically rare) |
| Recovery Time | Generally faster, often within a few days or weeks | Longer recovery period, typically several weeks |
| Costs | Potentially lower initial cost, but long-term costs may need further study | Higher upfront costs |
The comparison table provides a simplified overview. Specific success rates, complications, and recovery times can vary significantly based on individual patient factors, treatment specifics, and the expertise of the medical team.
Advantages of Non-Surgical Approaches
Non-surgical approaches offer the advantages of less invasiveness, shorter recovery periods, and often lower costs compared to surgery. Furthermore, the reduced risk of complications is a key driver for many patients choosing these alternatives. For instance, patients can return to their daily activities more quickly and with minimal discomfort, contributing to a better quality of life.
Disadvantages of Non-Surgical Approaches
Potential disadvantages of non-surgical treatments may include a slightly lower success rate in severe cases compared to surgery, and the need for ongoing follow-up and potentially repeated treatments. The availability and cost-effectiveness of these treatments may also vary geographically.
Advantages of Surgical Procedures
Surgical procedures, such as fundoplication, offer a more definitive resolution of GERD, potentially providing long-term symptom control in appropriate cases. This approach may be superior for cases of severe or persistent reflux.
Recent advancements in medical technology, particularly in 2023, are offering promising new ways to treat conditions like GERD without resorting to surgery. Exploring the latest innovations in new medical technology 2023 reveals exciting possibilities for less invasive GERD treatments. These developments are paving the way for more effective and less disruptive solutions for patients.
Disadvantages of Surgical Procedures
Disadvantages of surgical procedures include a longer recovery period, higher costs, and a greater risk of potential complications. Moreover, patients may experience post-operative discomfort and potentially require ongoing follow-up.
Last Word
In conclusion, the advancements in non-surgical GERD treatments offer a promising alternative to traditional approaches. While further research and clinical trials are crucial to fully validate these technologies, the potential for improved patient outcomes, reduced invasiveness, and potentially lower costs is substantial. This new era of GERD management necessitates careful consideration of potential risks, ethical implications, and patient preferences to ensure responsible and effective implementation.
FAQ
What are the common side effects of current GERD medications?
Some common side effects include nausea, headache, and constipation. Individual responses vary.
How long does it typically take for new technologies to receive regulatory approval?
The timeframe for regulatory approval varies depending on the specific technology and the regulatory body involved, but it often involves several years of rigorous testing and clinical trials.
What are some potential risks associated with these new technologies?
Potential risks will vary depending on the specific technology. Rigorous testing is essential to minimize these risks. Possible side effects and long-term consequences will be explored in the article.
What is the estimated cost comparison between surgical and non-surgical GERD treatments?
A detailed cost analysis of the different approaches will be presented, comparing the initial costs, long-term expenses, and overall cost-effectiveness of each.






